Newborn Care
- Vitamin K IM
- Prophylactic eye erythromycin
- Umbilical cord care
- Hearing test
- Newborn screening tests
Common Injuries During Deliveries
| Injury | Specifics | Outcome |
| Skull fractures | In utero from pressure against bones or forceps; linear: most common | • Linear: no symptoms and no treatment needed
• Depressed: elevate to prevent cortical injury |
| Brachial palsy | Erb-Duchenne: C5–C6; cannot abduct shoulder; externally rotate and supinate forearm; Klumpke: C7–C8 ± T1; paralyzed hand ± Horner syndrome | Most with full recovery (months); depends on whether nerve was injured or lacerated; Rx: proper positioning and partial
immobilization; massage and range of motion exercises; if no recovery in 3–6 mo, then neuroplasty |
| Clavicular fracture | Especially with shoulder dystocia in vertex position and arm extension in breech | Palpable callus within a week; Rx: with immobilization of arm and shoulder |
| Facial nerve palsy | Entire side of face with forehead; forceps delivery or in utero pressure over facial nerve | Improvement over weeks (as long as fibers were not torn); need eye care; neuroplasty if no improvement (torn fibers) |
| Caput succedaneum | Diffuse edematous swelling of soft tissues of scalp; crosses suture lines | Disappears in first few days; may lead to molding for weeks |
| Cephalohematoma | Subperiosteal hemorrhage: does not cross suture lines | May have underlying linear fracture; resolve in 2 wk to 3 mo; may calcify; jaundice |
Note:
- caput succedaneum (caput = cap over; succed = continuous); caphalohematoma = bleeding subperiosteum (stay in bone border)
- most trauma need only follow up
Physical Examination—Common Findings (see remaining chapter for other specific findings)
| Finding/Diagnosis | Description/Comments |
| Skin | |
| Cutis marmorata (pix) | Lacy, reticulated vascular pattern over most of body when baby is cooled; improves over first month; abnormal if persists |
| Milia | Firm, white papules; inclusion cyst; on palate midline: Epstein pearls; spontaneous resolution |
| Salmon patch (nevus simplex) (pix) | Pale, pink vascular macules; found in nuchal area, glabella, eyelids; usually disappears |
| Mongolian spots | Blue to slate-gray macules; seen on presacral, back, posterior thighs; > in nonwhite infants; arrested melanocytes; usually fade over first few years; differential: child abuse |
| Erythema toxicum neonatorum (pix) | Firm, yellow-white papules/pustules with erythematous base; peaks on second day of life; contain eosinophils; benign |
| Hemangioma | Superficial: bright red, protuberant, sharply demarcated; most often appear in first 2 months; most on face, scalp, back, anterior chest; rapid expansion, then stationary, then involution (most by 5–9 years of age); deeper: bluish hue, firm, cystic, less likely to regress; Rx: (steroids, pulsed laser) only if large and interfering with function |
| Neonatal acne | Erythematous papules on face; high maternal androgens; no treatment |
| Head | |
| Preauricular tags/pits (pix) | Look for hearing loss and genitourinary anomalies. |
| Coloboma of iris (pix) | Cleft at “six o’clock” position; most with other eye abnormalities; CHARGE association |
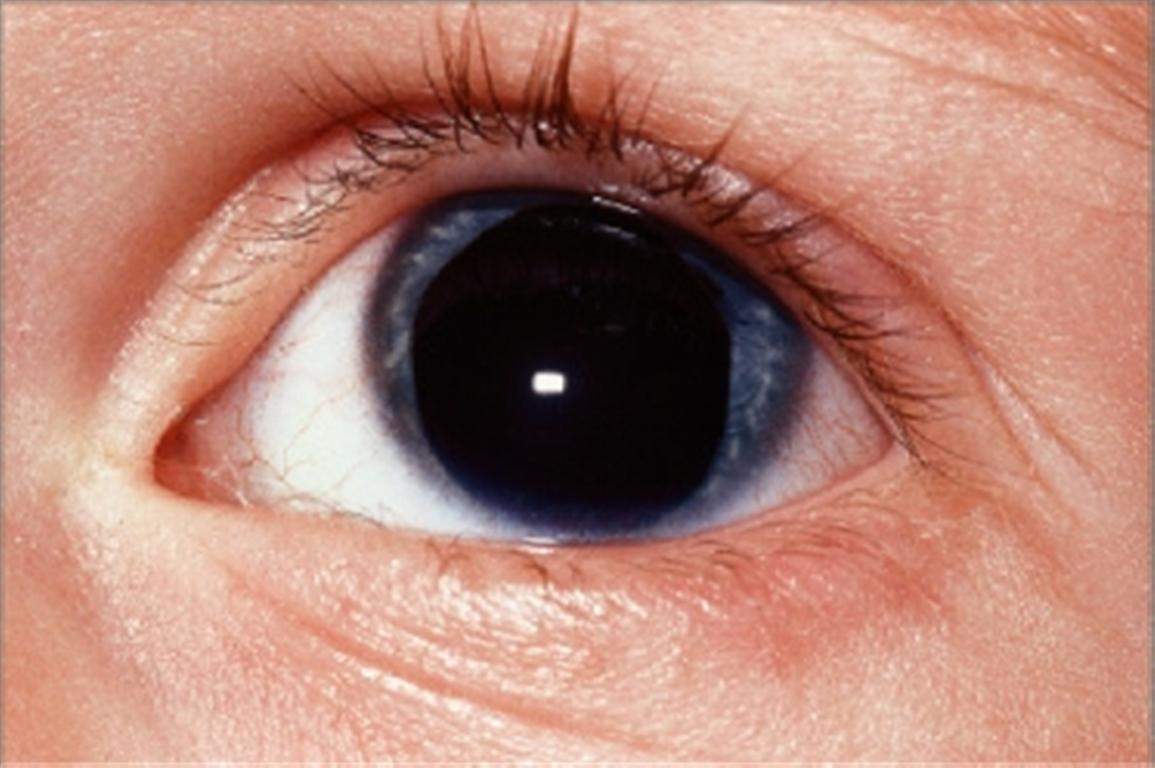
| Aniridia (pix) | Hypoplasia of iris; defect may go through to retina; association with Wilms tumor |
| Extremities | |
| Syndactyly | Fusion of fingers or toes. Get x-ray first for surgical planning. |
| Polydactyly
Finger tag |
>5 number of fingers or toes. No treatment needed if good blood supply.
Thin stalk, poor circulation; tie off at base → autoamputation |





NEWBORN SCREENING
Newborn Screening
- Every newborn before discharge or day 4 of life
- More reliable if done after 48 hours of oral feedings (substrates for metabolic diseases)
- Total diseases screened are determined by individual Some examples:
− Phenylketonuria
− Galactosemia
− Hypothyroidism
− Hb SS
− Cystic fibrosis
− Hb C
− Tyrosinemia
− 21-hydroxylase deficiency
Comparison of Two Newborn Screening Diseases*
| Phenylketonuria (PKU) | Classic Galactosemia | |
| Defect | Phenylalanine hydroxylase; accumulation of PHE in body fluids and CNS | Gal-1-P uridylyltransferase deficiency; accumulation of gal-1-P with injury to kidney, liver, and brain |
| Presentation | Mental retardation, vomiting, growth retardation, purposeless movements, athetosis, seizures | Jaundice (often direct), hepatomegaly, vomiting, hypoglycemia, cataracts, seizures, poor feeding, poor weight gain, mental retardation |
| Associations | Fair hair, fair skin, blue eyes, tooth abnormalities, microcephaly | Predisposition to E. coli sepsis; developmental delay, speech disorders, learning disabilities |
| Other comments | Normal at birth; gradual MR over first few months | May begin prenatally— transplacental galactose from mother |
| Treatment | Low PHE diet for life | No lactose—reverses growth failure, kidney and liver
abnormalities and cataracts, but not neurodevelopmental problems |
FETAL GROWTH AND MATURITY
Intrauterine Growth Restriction (IUGR)
| Type | Reason | Main Etiologies | Complications |
| Symmetric | Early, in utero insult that affects growth of most organs | Genetic syndromes, chromosomal abnormalities, congenital infections, teratogens, toxins | Etiology dependent; delivery of oxygen and nutrients to vital organs usually normal |
| Asymmetric (head sparing) | Relatively late onset after fetal organ development; abnormal delivery of nutritional substances and oxygen to the fetus | Uteroplacental insufficiency secondary to maternal diseases (malnutrition, cardiac, renal, anemia) and/or placental dysfunction (hypertension, autoimmune disease, abruption) | Neurologic (asphyxia) if significant decreased delivery of oxygen to brain |
Gestational Age and Size at Birth
| Preterm | Large for Gestational Age (LGA)—Fetal Macrosomia | Post-term |
| • Premature—liveborn infants delivered prior to 37 weeks as measured from the first day of the last menstrual period
• Low birth weight— birthweight ≤2,500 grams. This may be due to prematurity, IUGR, or both |
• Birth weight >4,500 grams at term
• Predisposing factors: obesity, diabetes • Higher incidence of birth injuries and congenital anomalies |
• Infants born after 42 weeks’ gestation from last menstrual period
• When delivery is delayed ≥3 weeks past term, significant increase in mortality. • Characteristics − Increased birth weight − Absence of lanugo − Decreased/absent vernix − Desquamating, pale, loose skin − Abundant hair, long nails − If placental insufficiency, may be meconium staining |
