Review – Kaplan Pediatrics: Growth & Nutrition
Basic Principles of Growth
- A newborn typically loses up to 10% of birth weight (BW) in the first week of life due to elimination of large amount of extravascular. Should regain or surpass BW by 2 weeks.
- A neonate should gain about 30 grams (1 oz) per day in the first month of life, which slows to about 20 grams/day at 3–4
- An infant typically doubles BW by 6 months and triples by 1 year.
- Growth rate slows further between 6 and 12 months and then appetite begins to decline through 18 months of age.
- Then height and weight increase at a steady rate, but head-circumference rate of growth decreases somewhat (2–5 years).
- Between 6 and 12 years: 3–6 growth spurts each year for 8-week periods each; slower brain growth; myelination complete by age 7
- Between 10 and 20 years: acceleration in early Boys’ highest growth stops at age 18. Their average peak is 13.5 years (2–3 years later than girls, and continues 2–3 years after girls have stopped). Girls’ average peak is 11.5 years and it stops at age 16.
Growth Patterns
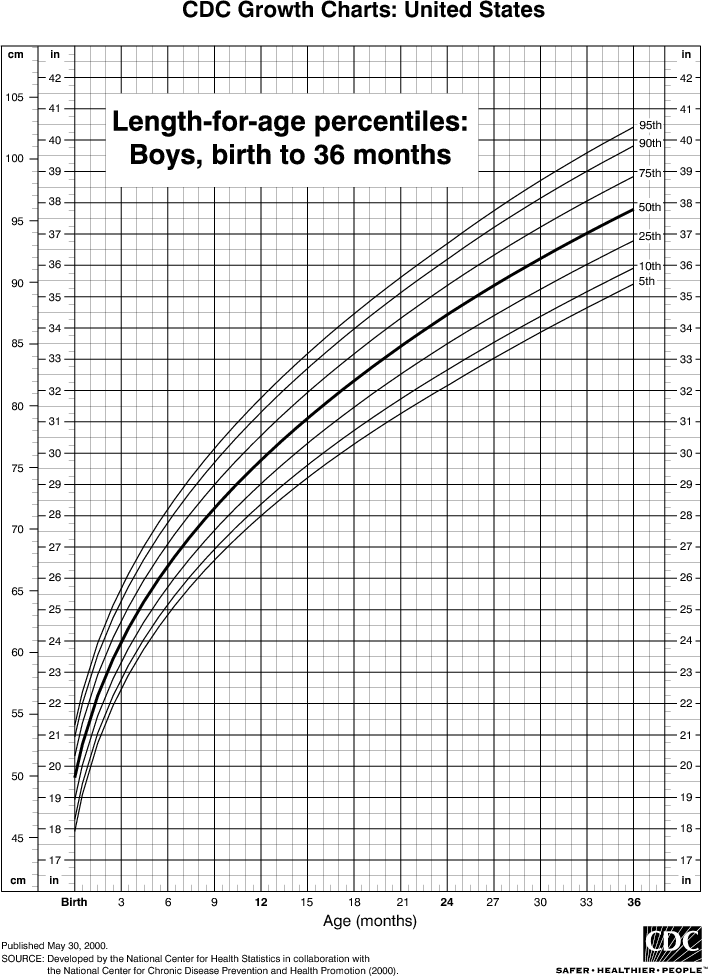
- Growth chart is the best tool to determine patterns of growth.
- Separate growth charts for boys and girls; charts measure weight for age, height for age, head circumference for age, weight for height, and body mass index (BMI).
- Each chart has multiple curves (either 5–95% or 3–97%).
EVALUATION OF GROWTH
Definitions
- Growth velocity (GV)—yearly increments of growth; should follow a growth curve slope = change in height : change in age
- Chronologic age (CA)—actual age
- Bone age (BA)—x-ray of left hand and wrist (non-dominant hand)
Short stature
- BA < CA
- Normal GV: constitutional delay
- Abnormal GV: chronic illness, nutritional deficiencies, endocrine disorders
- BA = CA
- Normal GV: familial short stature
- Abnormal GV: genetic syndromes associated with short stature
Tall stature
- BA ≥ CA
- Normal GV: familial tall stature, obesity
- Abnormal GV: genetic syndromes, endocrine disorders, CNS lesions
Table 3-1. Growth Velocity
| Normal | Abnormal | |
| Bone age = Chronological age | Ideal
Genetic (familial) short stature |
• Genetic
• Chromosomal |
| Bone age < Chronological age | Constitutional delay | • Chronic systemic disease
• Endocrine related |
| Bone age ≥
Chronological age |
Obesity (tall) Familial tall stature | • Precocious puberty
• Congenital adrenal hyperplasia • Hyperthyroidism |


Assessment of Growth
- Child is genetically programmed to stay on one to two growth curves after age 2
- Height percentile at 2 years of age correlates with final adult height percentile.
- Low-birth-weight and very-low-birth-weight infants may continue to show catch-up growth through early school age.
- Weight/height <5th percentile is the single best growth curve indicator for acute malnutrition. In nutritional insufficiency, weight decreases before length, and weight/height is low. For causes of decreased linear growth, length decreases first or at the same time as weight (e.g., GH deficiency).
- BMI is accepted as best clinical indicator for measure of under- and overweight.
- For bone age-reference standards, use radiographs of left hand and Skeletal maturity is linked more to sexual maturity than chronologic age.
FEEDING
- Normal newborn has sufficient stores of iron to meet requirements for 4–6 months, but iron stores and absorption are Breast milk has less iron than most formu- las, but has higher bioavailability.
- Formula is supplemented with vitamin D; breast fed must be supplemental from birth (400 IU/d).
- Vitamin K routinely is given IM (intramuscularly) at birth, so do not need supplementation.
- Breast milk and formula are 90% H20, so no additional H2O needs to be given
BREAST FEEDING
- General
- Most can breast feed immediately after birth and all can feed by 4–6 months
- Feeding schedule should be by self-regulation; most establish by 1 month
- Advantages
- Psychological/emotional—maternal-infant bonding
- Premixed; right temperature and concentration
- Immunity—protective effects against enteric and other pathogens; less diarrhea, intestinal bleeding, spitting up, early unexplained infant crying, atopic derma- titis, allergy, and chronic illnesses later in life; passive transfer of T-cell immunity
- Decreased allergies compared to formula fed
- Maternal—weight loss and faster return to preconceptional uterine size
- Contraindications
- HIV
- CMV, HSV (if lesions on breast)
- HBV (see note)
- Acute maternal disease if infant does not have disease (tuberculosis, sepsis)
- Breast cancer
- Substance abuse
- Drugs:
Absolute contraindications: ° Relative contraindications:
} Antineoplastics } Neuroleptics
} Radiopharmaceuticals } Sedatives
} Ergot alkaloids } Tranquilizers
} Iodide/mercurials } Metronidazole
} Atropine } Tetracycline
} Lithium } Sulfonamides
} Chloramphenicol } Steroids
} Cyclosporin
} Nicotine
} Alcohol
-
- Breast feeding is not contraindicated in mastitis
Comparison of Breast Milk to Cow Milk
| Component | Human Milk | Cow Milk |
| Water/solids | Same | Same |
| Calories | 20 cal/oz | 20 cal/oz |
| Protein | 1–1.5% (whey dominant) | 3.3% (casein dominant) |
| Carbohydrate | 6.5–7% lactose | 4.5% lactose |
| Fat | high in LCFAs | high in MCFAs |
| Minerals | Iron better absorbed | Low iron and copper |
| Vitamins | Diet dependent, low in K | Low in C, D |
| Digestibility | Faster emptying | Same after 45 days |
| Renal solute load | Low (aids in renal function) | Higher |
Do not give cow milk prior to one year of age
Formula Feeding
- Infant Formula feeding is used as a substitute for or to supplement breast milk. Most commercial formulas are cow-milk–based with modifications to approximate breast milk. They contain 20 calories/ounce. Specialty formulas (soy, lactose- free, premature, elemental) are modified to meet specific needs.
- Formula versus cow milk—Fe-deficiency anemia with early introduction (<1 yr) of cow’s
- Advanced feeding—Stepwise addition of foods (one new food every 3-4 days)
SOLIDS
- Iron-fortified cereal only at 4-6 months
- Step-wise introduction of strained foods (vegetables and fruits), then dairy, meats (6-9 months; stage I and II)
- Foods better saved for year 2:
- Egg whites
- Chocolate
- Nuts
- Citrus
- Wheat products
- Fish
- No honey in first year of life—infant botulism
DISORDERS OF GROWTH
Short stature
- Constitutional growth delay – child is short prior to onset of delayed adolescent growth spurt; parents are of normal height; normal final adult height is reached; growth spurt and puberty are delayed; bone age delayed compared to chronological age.
- Familial short stature – patient is parallel to growth curve; strong family history of short stature; chronologic age equals bone age
- Pathologic short stature – patient may start out in normal range but then starts cross- ing growth Differential diagnosis: craniopharyngioma, hypothyroidism, hypopituitarism, nutritional problems, and other chronic illnesses.
Tall stature
- Usually a normal variant (familial tall stature)
- Other causes – exogenous obesity, endocrine causes (growth hormone excess [gigan- tism, acromegaly], androgen excess [tall as children, short as adults)
- Syndromes – homocystinuria, Sotos, Klinefelter
Organic failure to thrive
- Malnutrition
- Initial diagnostic tests (when organic causes are suspected)- document caloric intake, CBC, urinalysis, liver function tests, serum protein, sweat chloride, stool for ova and parasites
Non-organic failure to thrive
- Child (usually infant) not fed adequate calories
- Emotional or maternal deprivation concurrent with nutritional deprivation
- Leads to neglect of infant; psychosocial deprivation most common reason in all age groups
- Other factors: retarded or emotionally disturbed parents; poverty
- Clinical findings
- Thin extremities, narrow face, prominent ribs, wasted buttocks
- Neglect of hygiene
- A flat occiput and hair loss may indicate excessive back-lying
- Delays in social and speech development
- Avoidance of eye contact, expressionless, no cuddling response
- Feeding aversions
- Diagnosis – Feed under supervision (may need hospitalization) for 1
- Should gain >2 oz/24 hours over the week
- May have a ravenous appetite
- Careful observations of mother; may need videotape
- Delay extensive lab evaluations until after dietary management has been attempted for 1 week and has failed
- Management
- All cases caused by underfeeding from maternal neglect must be reported to CPS
- Infants discharged to natural home require intensive and long-term intervention
- Feed, as above; usually require greater calories for catch-up May need NG feedings or even gastrostomy tube in severe cases
Obesity
- Risk factors – predisposition, parental obesity, family/patient inactivity, feeding baby as response to any crying, and rarely associated in syndromes (Prader-Willi; Down)
- Presentation – tall stature in some, abdominal striae, associated obesity of extremities; increased adipose tissue in mammary tissue in boys, large pubic fat pad, early puberty
- Diagnostic tests
- BMI >95% for age and sex is diagnostic of obesity
- 85 to 95% = overweight
- Complications – Obese infants and children are at increased risk of becoming obese adults (the risk is greater with advanced age of onset); cardiovascular (hypertension, increased cholesterol), hyperinsulinism, slipped capital femoral epithesis, sleep apnea, type 2 diabetes, acanthosis
- Treatment – exercise and balanced diet; no medications
