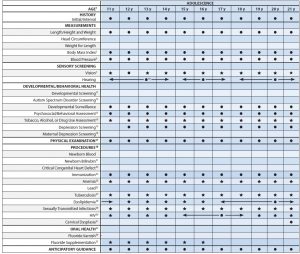
Bright Futures/AAP Recommendations for Preventive
Pediatric Health Care (Periodicity Schedule)
- Each child and family is unique; therefore, these Recommendations for Preventive Pediatric Health Care are designed for the care of children who are receiving competent parenting, have no manifestations of any important health problems, and are growing and developing in a satisfactory fashion. Developmental, psychosocial, and chronic disease issues for children and adolescents may require frequent counseling and treatment visits separate from preventive care visits. Additional visits also may become necessary if circumstances suggest variations from normal.
- These recommendations represent a consensus by the American Academy of Pediatrics (AAP) and Bright Futures. The AAP continues to emphasize the great importance of continuity of care in comprehensive health supervision and the need to avoid fragmentation of care.
- Refer to the specific guidance by age as listed in the Bright Futures Guidelines (Hagan JF, Shaw JS, Duncan PM, eds. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. 4th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2017).
- The recommendations in this statement do not indicate an exclusive course of treatment or standard of medical care. Variations, taking into account individual circumstances, may be appropriate. Copyright © 2019 by the American Academy of Pediatrics, updated March 2019.
- No part of this statement may be reproduced in any form or by any means without prior written permission from the American Academy of Pediatrics except for one copy for personal use.
Infancy
Early Childhood
Middle Childhood
Adolescence
1.
If a child comes under care for the first time at any point on the schedule, or if any items are not accomplished at the suggested age, the schedule should be brought up-to-date at the earliest possible time.
2.
A prenatal visit is recommended for parents who are at high risk, for first-time parents, and for those who request a conference. The prenatal visit should include anticipatory guidance, pertinent medical history, and a discussion of benefits of breastfeeding and planned method of feeding, per “The Prenatal Visit” (http://pediatrics.aappublications.org/content/124/4/1227.full).
3.
Newborns should have an evaluation after birth, and breastfeeding should be encouraged (and instruction and support should be offered).
4.
Newborns should have an evaluation within 3 to 5 days of birth and within 48 to 72 hours after discharge from the hospital to include evaluation for feeding and jaundice. Breastfeeding newborns should receive formal breastfeeding evaluation, and their mothers should receive encouragement and instruction, as recommended in “Breastfeeding and the Use of Human Milk” (http://pediatrics.aappublications.org/content/129/3/e827.full). Newborns discharged less than 48 hours after delivery must be examined within 48 hours of discharge, per “Hospital Stay for Healthy Term Newborns” (http://pediatrics.aappublications.org/content/125/2/405.full).
5.
Screen, per “Expert Committee Recommendations Regarding the Prevention, Assessment, and Treatment of Child and Adolescent Overweight and Obesity: Summary Report” (http://pediatrics.aappublications.org/content/120/Supplement_4/S164.full).
6.
Screening should occur per “Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents” (http://pediatrics.aappublications.org/content/140/3/e20171904). Blood pressure measurement in infants and children with specific risk conditions should be performed at visits before age 3 years.
7.
A visual acuity screen is recommended at ages 4 and 5 years, as well as in cooperative 3-year-olds. Instrument-based screening may be used to assess risk at ages 12 and 24 months, in addition to the well visits at 3 through 5 years of age. See “Visual System Assessment in Infants, Children, and Young Adults by Pediatricians” (http://pediatrics.aappublications.org/content/137/1/e20153596) and “Procedures for the Evaluation of the Visual System by Pediatricians”(http://pediatrics.aappublications.org/content/137/1/e20153597).
8.
Confirm initial screen was completed, verify results, and follow up, as appropriate. Newborns should be screened, per “Year 2007 Position Statement: Principles and Guidelines for Early Hearing Detection and Intervention Programs” (http://pediatrics.aappublications.org/content/120/4/898.full).
9.
Verify results as soon as possible, and follow up, as appropriate.
10.
Screen with audiometry including 6,000 and 8,000 Hz high frequencies once between 11 and 14 years, once between 15 and 17 years, and once between 18 and 21 years. See “The Sensitivity of Adolescent Hearing Screens Significantly Improves by Adding High Frequencies” (http://www.jahonline.org/article/S1054-139X(16)00048-3/fulltext).
11.
See “Identifying Infants and Young Children With Developmental Disorders in the Medical Home: An Algorithm for Developmental Surveillance and Screening” (http://pediatrics.aappublications.org/content/118/1/405.full).
12.
Screening should occur per “Identification and Evaluation of Children With Autism Spectrum Disorders” (http://pediatrics.aappublications.org/content/120/5/1183.full).
13.
This assessment should be family centered and may include an assessment of child social-emotional health, caregiverdepression, and social determinants of health. See “Promoting Optimal Development: Screening for Behavioral and Emotional Problems” (http://pediatrics.aappublications.org/content/135/2/384) and “Poverty and Child Health in the United States” (http://pediatrics.aappublications.org/content/137/4/e20160339).
14.
A recommended assessment tool is available at http://crafft.org.
15.
Recommended screening using the Patient Health Questionnaire (PHQ)-2 or other tools available in the GLAD-PC toolkit and at http://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Mental-Health/Documents/MH_ScreeningChart.pdf. )
16. Screening should occur per “Incorporating Recognition and Management of Perinatal and Postpartum Depression Into Pediatric Practice” (http://pediatrics.aappublications.org/content/126/5/1032).
17.
At each visit, age-appropriate physical examination is essential, with infant totally unclothed and older children undressed and suitably draped. See “Use of Chaperones During the Physical Examination of the Pediatric Patient” (http://pediatrics.aappublications.org/content/127/5/991.full).
18.
These may be modified, depending on entry point into schedule and individual need.
19.
Confirm initial screen was accomplished, verify results, and follow up, as appropriate. The Recommended Uniform Screening Panel (https://www.hrsa.gov/advisory-committees/heritable-disorders/rusp/index.html), as determined by The Secretary’s Advisory Committee on Heritable Disorders in Newborns and Children, and state newborn screening laws/regulations (http://genes-r-us.uthscsa.edu/home) establish the criteria for and coverage of newborn screening procedures and programs.
20.
Verify results as soon as possible, and follow up, as appropriate.
21.
Confirm initial screening was accomplished, verify results, and follow up, as appropriate. See “Hyperbilirubinemia in the Newborn Infant ≥35 Weeks’ Gestation: An Update With Clarifications” (http://pediatrics.aappublications.org/content/124/4/1193).
22.
Screening for critical congenital heart disease using pulse oximetry should be performed in newborns, after 24 hours of age, before discharge from the hospital, per “Endorsement of Health and Human Services Recommendation for Pulse Oximetry Screening for Critical Congenital Heart Disease” (http://pediatrics.aappublications.org/content/129/1/190.full).
23.
Schedules, per the AAP Committee on Infectious Diseases, are available at http://redbook.solutions.aap.org/SS/Immunization_Schedules.aspx. Every visit should be an opportunity to update and complete a child’s immunizations.
24.
Perform risk assessment or screening, as appropriate, per recommendations in the current edition of the AAP Pediatric Nutrition: Policy of the American Academy of Pediatrics (Iron chapter).
25.
For children at risk of lead exposure, see “Prevention of Childhood Lead Toxicity” (http://pediatrics.aappublications.org/content/138/1/e20161493) and “Low Level Lead Exposure Harms Children: A Renewed Call for Primary Prevention” (http://www.cdc.gov/nceh/lead/ACCLPP/Final_Document_030712.pdf).
26.
Perform risk assessments or screenings as appropriate, based on universal screening requirements for patients with Medicaid or in high prevalence areas.
27.
Tuberculosis testing per recommendations of the AAP Committee on Infectious Diseases, published in the current edition of the AAP Red Book: Report of the Committee on Infectious Diseases. Testing should be performed on recognition of high-risk factors.
28.
See “Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents” (http://www.nhlbi.nih.gov/guidelines/cvd_ped/index.htm).
29.Adolescents should be screened for sexually transmitted infections (STIs) per recommendations in the current edition of the AAP Red Book: Report of the Committee on Infectious Diseases.
30.Adolescents should be screened for HIV according to the USPSTF recommendations (http://www.uspreventiveservicestaskforce.org/uspstf/uspshivi.htm) once between the ages of 15 and 18, making every effort to preserve confidentiality of the adolescent. Those at increased risk of HIV infection, including those who are sexually active, participate in injection drug use, or are being tested for other STIs, should be tested for HIV and reassessed annually.
31.See USPSTF recommendations (https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/cervical-cancer-screening2). Indications for pelvic examinations prior to age 21 are noted in “Gynecologic Examination for Adolescents in the Pediatric Office Setting” (http://pediatrics.aappublications.org/content/126/3/583.full).
32.Assess whether the child has a dental home. If no dental home is identified, perform a risk assessment (https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Oral-Health/Pages/Oral-Health-Practice-Tools.aspx) and refer to a dental home. Recommend brushing with fluoride toothpaste in the proper dosage for age. See “Maintaining and Improving the Oral Health of Young Children” (http://pediatrics.aappublications.org/content/134/6/1224).
33.Perform a risk assessmentSee “Maintaining and Improving the Oral Health of Young Children” (http://pediatrics.aappublications.org/content/134/6/1224).
34.See USPSTF recommendations (https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/dental-caries-in-children-from-birth-through-age-5-years-screening). Once teeth are present, fluoride varnish may be applied to all children every 3–6 months in the primary care or dental office. Indications for fluoride use are noted in “Fluoride Use in Caries Prevention in the Primary Care Setting” (http://pediatrics.aappublications.org/content/134/3/626).
35.If primary water source is deficient in fluoride, consider oral fluoride supplementation. See “Fluoride Use in Caries Prevention in the Primary Care Setting” (http://pediatrics. aappublications.org/content/134/3/626).
Summary of Changes Made to the
Bright Futures/AAP Recommendations for Preventive Pediatric Health Care
(Periodicity Schedule)
This schedule reflects changes approved in December 2018 and published in March 2019. For updates and a list of previous changes made, visit www.aap.org/periodicityschedule.
CHANGES MADE IN DECEMBER 2018
BLOOD PRESSURE
••
Footnote 6 has been updated to read as follows: “Screening should occur per ‘Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents’ (http://pediatrics.aappublications.org/content/140/3/e20171904). Blood pressure measurement in infants and children with specific risk conditions should be performed at visits before age 3 years.”
ANEMIA
••
Footnote 24 has been updated to read as follows: “Perform risk assessment or screening, as appropriate, per recommendations in the current edition of the AAP Pediatric Nutrition: Policy of the American Academy of Pediatrics (Iron chapter).”
LEAD
••
Footnote 25 has been updated to read as follows: “For children at risk of lead exposure, see ‘Prevention of Childhood Lead Toxicity’ (http://pediatrics.aappublications.org/content/138/1/e20161493) and ‘Low Level Lead Exposure Harms Children: A Renewed Call for Primary Prevention’ (https://www.cdc.gov/nceh/lead/ACCLPP/Final_Document_030712.pdf).”