Long-term management of panic attacks
Câu 1. A 50-year-old African American woman comes to the primary care provider’s office because of panic attacks over the past two months. She reports a recent incident in which she began experiencing palpitations, tachycardia, cold sweats, trembling, dizziness, and an overwhelming fear of death while she was riding on a public bus. She reports similar incidents at work and the grocery store. She is now terrified about these attacks and concerned that they will interfere with her work. Her temperature is 38°C (100.4°F); pulse is 70/min; respirations are 18/min, and blood pressure is110/60 mm Hg. Serum catecholamines, thyroid function test, vitamin B12, serum glucose, and a complete blood count results are ordered and return within normal limits. She states that she is not interested in cognitive behavioral therapy. Which of the following is the next appropriate step in long-term management of the patient’s condition?
Benzodiazepines
Benzodiazepines act on the γ-aminobutyric acid (GABA) A receptor to enhance the effect of GABA on the central nervous system. This not only acts as an anticonvulsant but also causes hypnosis and anxiolysis. Benzodiazepines are effective for acute anxiolysis. However, long term use can lead to dependence and addiction.
Buproprion
Buproprion is a re-uptake inhibitor of norepinephrine and dopamine. It is used to treat patients with major depressive disorder and tobacco abuse. Bupropion will not cause weight gain and sexual dysfunction. It can cause seizures in patients witheating disorders.
Sertraline
Major takeaway
Patients with panic disorder will experience panic attacks and will excessively worry about these panic attacks. Treat these patients with a selective serotonin re-uptake inhibitor such as sertraline.
Main explanation
Panic attacks are episodes in which patients can experience symptoms such as palpitations, abdominal distress, nausea, chills, chest pain, diaphoresis, shortness of breath, and a fear of death. These episodes can last anywhere between 10 to 25 minutes. These panic attacks can be triggered by a specific event or occur spontaneously. Before panic disorder can be diagnosed, other medical causes of anxiety need to be ruled out including hyperthyroidism, vitamin B12 deficiency, anemia, pheochromocytoma, hypoglycemia, medications, and illicit substance abuse.
Patients with panic disorder will experience panic attacks and will excessively worry about these panic attacks. Panic disorder can be characterized as with or without agoraphobia. Agoraphobia refers to fear in public locations in which it is difficult to escape. Examples include being on a bus or in a tightly crowded elevator.
First-line treatment for panic disorder is a selective serotonin re-uptake inhibitor. Benzodiazepines can be utilized on an “as needed” basis. However, it is not an optimal for long term control as chronic benzodiazepine use can induce dependence in the patient. Sertraline is a serotonin re-uptake inhibitor and hence increase concentrations of serotonin within the synaptic cleft.
Selegiline
Selegiline is a monoamine oxidase inhibitor which is used to treat depression. Patients on selegiline need to carefully monitor tyramine uptake and avoid curedmeats and red wine. Selegiline will not have effects on insomnia and weight gain
Thyroxine
Thyroxine is a thyroid replacement medication used to treat patients with hypothyroidism. Patients taking thyroxine with acute episodes of anxiety should have a thyroid function test ordered as iatrogenic hyperthyroidism can lead to panic attacks.
Psychology of patient-physician relationship
Câu 2. A 42-year-old psychiatrist is excited to evaluate his new patient. While interviewing the patient, he realizes that the male patient’s story is very similar to his uncle’s, with whom he was very close during childhood. The patient reveals that he is addicted to cocaine. The psychiatrist starts remembering what he felt when his uncle died of a cocaine overdose. After awhile, the doctor starts feeling sorry for him and becomes very interested in helping the patient overcome his addiction by any means. What type of response is the doctor showing with this behavior towards the patient?
Counter-transference
Major takeaway
Transference would occur if the patient projects his own feelings towards a formative subject in his life to the physician. Counter-transference would occur if the physician projects his own feelings towards a formative subject in his life to his patient. Remember, paTient Transfers while physiCian Counter-transfers!
Main explanation
The psychiatrist is redirecting the feelings he had for his uncle, who died of a cocaine overdose, towards his patient who suffers cocaine addiction. Punishment and Extinction are related to Operant conditioning and are not related to this behavior. Transference would occur if the patient projects his own feelings towards an important person in his life to his psychiatrist.
An old man presenting with weight loss and early satiety
Câu 3. An 80-year-old Korean man comes to the office because of abdominal pain, weight loss, and early satiety. He says that he has been experiencing some discomfort in the mid-epigastrium. The pain started approximately a year ago, but he thought it was acid indigestion so he took a proton pump-inhibitor which alleviated his pain. The pain has since worsened and he is now experiencing dysphagia. He has lost 9.1-kg (20-lb) over the past 6 months, is easily fatigued, and unable to perform daily tasks around the house. He has a history of coronary artery disease and hypertension. Physical examination shows tenderness to deep palpation in the mid-epigastrium as well as cachexia. Laboratory findings include anemia with a hemoglobin of 8.0 g/dL and hematocrit of 24% with a mean corpuscular volume of 70 fL. A fecal occult blood test is positive. Which of the following is the most likely diagnosis?
Colon cancer
Colon cancer can cause a positive fecal occult blood test, cachexia and similar lab findings. However, dysphagia, and discomfort in the mid-epigastrium are not common. Changes in bowel habits and consistency of stools are common in colon cancer.
Gastric cancer
Major takeaway
Gastric cancer is generally asymptomatic until the cancer is at an advanced stage. In all elderly patients that have significant weight loss and a positive fecal occult blood test, the diagnosis is cancer until proven otherwise. Risk factors for gastric cancer include Helicobacter pyloriinfection, pernicious anemia, diet, and a positive family history.
Main explanation
The patient described has been diagnosed with gastric cancer. Patients that have gastric cancer are generally asymptomatic until their cancer is at an advanced stage. Typical signs and symptoms in patients who are symptomatic include weight loss, anorexia, dyspepsia, dysphagia, epigastric pain, and early satiety. The development of dysphagia is a common symptom for tumors that involve the proximal stomach or cardia. Some patients may also develop upper gastrointestinal bleeding resulting in hematemesis and/or a positive fecal occult blood test. Gastric cancer classically metastasizes to the supraclavicular lymph nodes (Virchow node), periumbilical lymph nodes (Sister Mary Joseph Nodule) and to the ovaryin women (Krukenburg tumor). These regions of metastasis are typical in advanced stages of gastric cancer. Gastric cancer is rare in the U.S., but is one of the most common cancers worldwide and is particularly common in Asians. Risk factors for gastric cancer include Helicobacter pylori infection, pernicious anemia, diet (high in nitrates, salt, fat), and a positive family history.
Gastric outlet obstruction
Gastric outlet obstruction is characterized by an obstruction at the gastric pylorus. Patients are generally characterized by recurrent non-bilious vomiting.
Peptic ulcer disease
Discomfort in the mid-epigastrium relieved by proton pump inhibitors is typical in peptic ulcer disease. Patients with peptic ulcer disease also have an exacerbation of symptoms following oral intake. The development of cachexia and dysphagia is uncommon.
Small bowel obstruction
Small bowel obstruction commonly causes bilious vomiting (early symptom), abdominal distention, constipation, hyperactive bowelsounds (high-pitched, rushing sounds), and usually poorly localized abdominal pain. Radiographs show multiple air-fluid levels.
An appropriate choice of long-term birth control for young girl
Câu 4. A 15 year old nulliparous woman makes an appointment at the gynecology clinic to obtain birth control. She has recently become sexually active with one male partner and does not desire children at this time. She does want to have children when she gets older. She tells you her older sister has an intrauterine device (IUD) for birth control and that she is interested in getting an intrauterine device too. The patient has no medical problems and has regular menstrual periods. Is an intrauterine device an appropriate choice of birth control for this patient?
No, the intrauterine device cannot be used in nulliparous women.
TWO
Yes, an intrauterine device is an appropriate choice of birth control for this patient.
Main explanation
The intrauterine device is an appropriate choice of birth control for this patient – a 15 year old (with no contraindications) requiring long-term contraception. Intrauterine devices may be used in nulliparous women and there is no age requirement for their use. Intrauterine deviceuse is not associated with an increased risk of pelvic inflammatory disease in nulliparous patients. There is also no association between intrauterine device use and subsequent infertility. This patient should be counseled to use or have her partner use condoms to prevent the transmission of sexually transmitted infections.
Major Takeaway:
IUDs provide long-term contraception and are not associated with subsequent infertility. They do not protect against STIs, so the patient + partner must continue to use barrier protection for that purpose.
No, the intrauterine device should not be used in women who desire future fertility.
TWO
No, the intrauterine device cannot be used in women under the age of 25.
TWO
Sharp, stabbing pain on side of face
Câu 5. A 55 year old, Caucasian female presents to the clinic with complaints of a sharp, stabbing pain on the left side of her face, which comes and goes intermittently. She denies any loss of sensation or tingling.
What is the drug of choice for her condition?
Carbamazepine
Main explanation
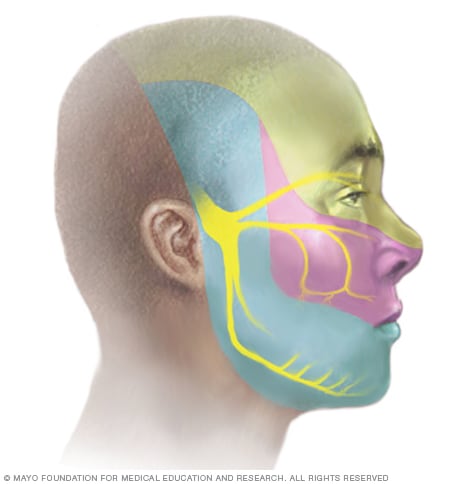
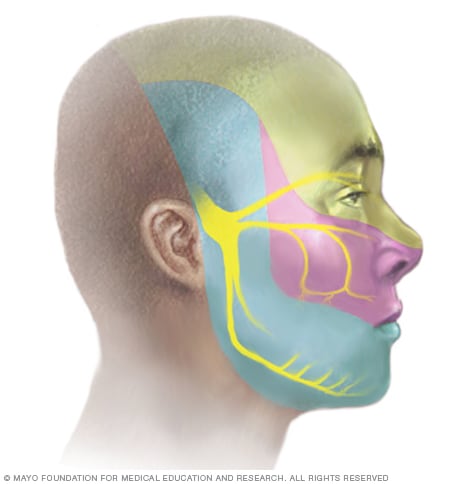
Carbamazepine is a tricyclic anti-convulsant drug related to imipramine. It is the drug of choice for treatment of idiopathic trigeminal neuralgia (trigeminal neuralgia occurring without any known cause).
Trigeminal neuralgia is characterized by recurrent paroxysms of sharp, stabbing pain in one or more branches of the trigeminal nerve, usually on one side of the face. It usually occurs after 50 years of age and is more common in women than in men.
Major takeaway:
Carbamazepine is the 1st line pharmacological treatment for trigeminal neuralgia.
A case of worsening coordination
Câu 6. A 42-year-old woman comes to the clinic because of worsening coordination. She says she often falls over, cannot button up her shirts, and has difficulty swallowing. Physical examination shows slightly slurred speech and intermittent repetitive, wide circular movements of her arms. Her daughter, who is present, tells you that her mother has also lost speed and flexibility in thinking. Most of the time she seems depressed and lately she has been quite difficult to get along with; persistently focusing on minutiae and perseverating on repetitive, superstitious behaviors. Which of the following genetic findings is most consistent with this presentation?
>40 CAG repeats in the HD gene
Major takeaway
Huntington disease is a neurodegenerative disease of the trinucleotide repeat (CAG) family. It is characterized by chorea, dementia, and personality/behavioral changes.
Main explanation
Huntington disease is an autosomal dominant, highly penetrant, degenerative disorder of the nervous system. It is characterized by:
• Chorea (incessant, rapid, jerky movements)
• Cognitive impairment (dementia)
• Personality and behavioral changes
• Death 15-20 years after the onset of symptoms
• Onset of disease 4th-5th decade of life
Huntington disease involves the death of neurons in the caudate nucleus, a part of the basal ganglia involved in regulating voluntary movement. The death of nerve cells in the caudate nucleus is thought to cause the chorea.
The Huntington Disease (HD) gene is located on chromosome 4; this gene encodes a protein called Huntingtin. The codon (CAG) that encodes glutamine is repeated 19-22 times in the normal gene but >40 times in the mutated gene.
Remember that in diseases that involve trinucleotide expansion each successive generation of a family that harbors the mutant gene manifests the disease with greater severity at an earlier age, this is called genetic anticipation.
>100 CTG repeats in the OSCA gene
This pattern occurs in spinocerebellar ataxia Type 8. Typically, patients with ataxia progressively lose physical control but maintain full mental capacity.
>100 GAA repeats in the FXN gene
This pattern occurs in Friedreich ataxia. This type of ataxia is characterized by degeneration of nervous tissue in the spinal cord. The behavioral changes seen in this patient are inconsistent with an ataxia diagnosis.
>200 CGG repeats in the FMR1 gene
This pattern occurs in Fragile X mental retardation. Cases of fragile X syndrome are caused by abnormal CGG repeats ranging as high as over 1,000 times.
>200 CTG repeats in the DMPK gene
This pattern occurs in Myotonic dystrophy type 1. Typical symptoms of myotonic dystrophy include hypersomnia and loss of executive function.
A neonate not passing any meconium
Câu 7. A neonate is born to a 40-year-old woman, gravida 1, para 0. The neonate has upslanting palpebral fissures and a flat facial profile. The child feeds well, but by the second day still has not passed any meconium. An abdominal X-ray is done, and the results are shown below. Which of the following is most likely to be found on rectal biopsy?

Aganglionosis
Major takeaway
Hirschsprung disease can cause meconium retention in newborns. Diagnosis is made with rectal biopsy, which shows complete absence of ganglionic cells.
Main explanation
This patient has not passed meconium in 2 days, and the abdominal radiograph shows a severely dilated colon. These findings are consistent with a diagnosis of Hirschsprung disease.
Hirschsprung disease occurs due to migration failure of neural crest cells. The aganglionicdistal colon cannot relax, and creates an obstruction. This results in failure to pass meconium, as well as a dilated colon proximal to the aganglionosis. Hirschsprung disease is more common in patients with Down syndrome; this patient was born to a mother >35 years of age with physical examination findings consistent with the trisomy. This correlation is explained in part by mutations in the Down syndrome cell adhesion molecule gene seen in patients with Down syndrome-associated Hirschsprung disease.
Crypt abscesses
Crypts abscesses are a classic finding of ulcerative colitis, a type of inflammatory bowel disease. This disease typically presents in early adulthood with bloody diarrhea, abdominal pain, and tenesmus.
Diverticula
Diverticula are sac-like outpouchings in the colonic wall and are a common finding in older adults. Diverticulosis may be asymptomatic or it may be characterized by rectal bleeding and progress to diverticulitis, an inflammatory condition. Meckel diverticulum is a congenital condition that presents in children with bright red rectal bleeding.
Pseudomembranes
Pseudomembranous colitis is most commonly caused by infection with C. difficile. It is typically found in healthcare settings and is characterized by watery diarrhea, abdominal pain with cramping, and a low-grade fever.
Unremarkable biopsy
This patient has Hirschsprung disease and therefore will show a lack of ganglionic cells on rectal biopsy. Irritable bowel syndromeis a diagnosis of exclusion and typically has unremarkable biopsy findings. It is rarely diagnosed in young children or neonates.
A patient presenting with progressive pain with swallowing after a recent trip to Africa
Câu 8. A 58-year-old woman comes to the urgent care clinic because of a several month history of progressive pain with swallowing. She has difficulties tolerating solids or liquids and also has foul-smelling breath. She has no known allergies and has recently traveled to South America. A barium swallow study is obtained and the results of which are shown below. Which of the following is the most appropriate next step in management for this patient?

Cricopharyngeal myotomy
A myotomy procedure involves severing muscle fibers to enhance relaxation. This patient is characterized by symptoms of lower esophageal constriction (not upper), so a cricopharyngeal myotomy would not be beneficial.
Fundoplication of the stomach
Fundoplication is a treatment for severe gastro-esophageal reflux disease. The procedure involves wrapping the fundus of the stomach around the lower end of the esophagus. This procedure aids in the closure of the lower esophageal sphincter, which would worsen this patient’s existing achalasia.
Gastric bypass surgery
Gastric bypass surgery is a surgical treatment for morbid obesity. In a Roux-en-Y bypass the stomach is transected and the proximal part is attached to the jejunum. This patient is not morbidly obese and would not benefit from the procedure.
Injection of botox into the lower esophageal sphincter
Major takeaway
The bird’s beak sign is indicative of achalasia. Achalasia is commonly treated with botoxinjections into the lower esophageal sphincter; however, the most effective treatment is a Heller myotomy.
Main explanation
The chest X-ray shows the characteristic bird-beak sign of achalasia. Achalasia is narrowing of the lower esophageal sphincter (LES) due to the destruction of the myenteric plexus. It can be idiopathic or secondary to a known insult, such as Trypanosoma cruzi. Achalasia is generally characterized by progressive dysphagia, foul breath, chronic cough, and regurgitation.Treatment of achalasia may involve botulinum injection of the LES. Botulinum toxin damages acetylcholine-releasing neurons, which leads to decreased levels of the neurotransmitter. This will lead to decreased contraction of the sphincter and at least partial relief of symptoms. Other treatment options for achalasia include pneumatic dilation of the LES or surgical myotomy.
Injection of botox into the upper esophageal sphincter
This patient is characterized by signs and symptoms of achalasia, defined as the loss of myenteric neurons in the lower esophageal sphincter. Botox injection into the upper esophageal sphincter would not be beneficial to this patient.
A psychiatric patient present with involuntary chewing movements, lip smacking, and grimacing
Câu 9. A 75-year-old woman comes to the clinic for a routine check-up. She has a long history of schizophrenia, requiring antipsychotictreatment on many various agents including risperidone and haldol. She denies a history of depression, suicidal ideation, homicidalideation, or illicit drug use. Physical examination shows involuntary chewing movements, lip smacking, and grimacing. She says these symptoms may have started about 2 months ago, but she thought it was just a sign of old age. Which of the following is the most likely diagnosis?
Acute dystonia
Acute dystonia involves twisting of the neck, trunk, and limbs into uncomfortable positions and usually occurs earlier in the course of treatment.
Akathisia
Akathisia is a common side-effect of antipsychotics. However, it is a movement disorder characterized by a sense of restlessness and inability to sit still.
Athetosis
Athetosis is a form of motor dysfunction characterized by slow, involuntary movements, fluctuations in muscle tone, and imbalance. It is often associated with cerebral palsy
Parkinsonism
Drug-induced parkinsonism is characterized by a resting tremor, increased rigidity, masked facies and other characteristics often seen in patients with Parkinson syndrome.
Tardive dyskinesia
Major takeaway
Tardive dyskinesia is characterized by repetitive, involuntary, purposeless movements that can include lip smacking, pursing of the lips, tongue movements, and grimacing. They develop after years of treatment with typical antipsychotics (typical>atypical), especially haloperidol. Clozapine, an atypical antipsychotic, is least likely to cause tardive dyskinesia.
Main explanation
The patient has classic signs of tardive dyskinesia, a neurological condition characterized by involuntary movements of the tongue, lips, face, trunk, and extremities. It most often occurs in patients undergoing long-term (>3 months) or high-dose treatments of antipsychotic medications – most notably dopaminergic antagonists.
Neuroleptic-induced tardive dyskinesia is characterized by choreiform, athetoid, and rhythmic movements of the tongue, jaw, trunk, and extremities that have persisted for at ≥4 weeks and that began during treatment with neuroleptics or within 4 weeks of discontinuing neuroleptics. Diagnosis of neuroleptic-induced TD generally requires exposure to neuroleptics for at ≥3 months. At least a month of exposure is typically required if the patient is aged 60 years or older. There is no effective treatment. Typical antipsychotics are more likely to cause tardive dyskinesia compared to atypical antipsychotics. If patients are particularly concerned about tardive dyskinesia, clozapine is the antipsychotic with the least likelihood of inducing the condition.
A young girl presenting with 2-month abdominal pain
Câu 10. An 8-year-old girl comes to the office because of abdominal pain for the last two months. She says the pain is constant and pressure-like, and is located in left lower quadrant. Her parents also report that she has had four episodes of urinary incontinence in the last month. She had previously had good control of her bladder. She has not begun menstruating. On examination she has Tanner stage 1 breast and pubic hair development. An ultrasound reveals a mass on her left ovary. Fine needle aspiration of the mass shows tubular spaces lined with flattened cuboidal cells as well as central vessels surrounded by invaginated papillary structures. Her serum alpha-fetoprotein (AFP) is elevated. What is the most likely diagnosis?
Endometriosis
Endometriosis is defined as endometrial glands and stroma that occur outside the uterine cavity. Endometriosis can be present on the ovary, often referred to as an endometrioma, or “chocolate cyst. They are unlikely to present in a girl that has not reached menarche.
Follicular cyst
A follicular cysts are due to the failure of a mature follicle to properly ovulate and involute. They are generally asymptomatic, unless bleeding or They are unlikely to present in a girl that has not reached menarche.
Teratoma
Teratomas are the most common type of germ cell tumor, they contain cells from multiple germ layers and most are most often benign. Most teratomas are cystic and composed of mature differentiated elements, also known as dermoid cysts.
Yolk sac tumor
Major takeaway
Yolk sac tumors are malignant germ cell ovarian tumors typically seen in young women. Patients commonly present with symptoms related to the presence of a pelvic mass. Histologically these tumors resemble the yolk sac, and a serum AFP is the most commonly elevated tumor marker. Schiller-Duval bodies may be seen.
Main explanation
Common symptoms of a pelvic mass include abdominal pain, pressure and urinary incontinence. The pain may be acute and may be misdiagnosed as appendicitis.
Yolk sac tumors make up 14-20% of all malignant ovarian germ cell neoplasms. Yolk sactumors are aggressive malignant tumors typically found in the ovaries of young women, and less commonly in the testes of young boys. Tumor growth if often rapid with extensive intraperitoneal dissemination.
Histologically these tumors resemble yolk sac tissue, with the presence of tubules lined by a simple cuboidal epithelium and may demonstrate papillary invaginations that surround a central vessel, which are known as Schiller-Duval bodies. Because of the similarity of this tissue to yolk sac tissue, serum alpha-fetoprotein (AFP) is usually elevated and can be used to determine response to treatment, and to monitor for tumor recurrence. Lactate dehydrogenaseLDH may also be elevated in yolk sac tumors, although this is less common
Dysgerminoma
Dysgerminomas represent 2% of ovarian neoplasms, but account for 33% of malignant ovarian germ cell tumors. Histologically dysgerminomas have the appearance of a “fried egg” with a large clear cytoplasm surrounding a central nuclei. Serum alpha-fetoprotein (AFP) is usually normal, human chorionic gonadotrophin (ß-hCG) and lactate dehydrogenase (LDH) are often elevated.