The average age at menopause in the United States is 51 years with a normal range from 40 to 58 years of age
Menopause
Aka: Menopause, Perimenopause, Postmenopause
II. Definition
- Physiologic transition to cessation of Ovulation and menstruation, and reduced ovarian endocrine function
III. Symptoms: Perimenopause (lasts 3-8 years)
- Disturbance in menstrual pattern
- Shorter menstrual interval
- Heavier menstrual flow
- Hot Flashes (50-75% of women)
- Worse with higher BMI, Tobacco use and black race
- Gold (2006) Am J Public Health 96(7): 1226-35 [PubMed]
- Atrophic conditions (responds to Estrogen)
- Vaginal Mucosa (Atrophic Vaginitis)
- Vaginitis or vaginal Pruritus
- Dyspareunia
- Urethritis
- Dysuria, urgency, or Urinary Frequency
- Recurrent Urinary Tract Infection
- Vaginal Mucosa (Atrophic Vaginitis)
- Neuropsychological changes
- Major Depression
- Insomnia
- Hippocampus changes
- Decreased memory
- Decreased learning
- Decreased navigation or way finding
- Testosterone Deficiency (worse in surgical Menopause)
- Decreased energy and sense of well being
- Decreased sexual desire, arousability, and orgasm
- Decreased clitoral sensitivity
- Decreased nipple sensitivity
- Thinning of pubic hair
IV. Labs
- Follicle Stimulating Hormone (FSH)
- Not necessary to confirm diagnosis
- May be indicated for perimenopausal women age <45
- FSH >25 mIU/ml confirms Perimenopause or Menopause
- Measure on any day if patient is not having Menses
- Measure on Day 3 of cycle in menstruating women
- Measure Day 6-7 of Oral ContraceptivePlacebo week
- Confirms Birth Control no longer needed
- Thyroid Stimulating Hormone (TSH)
- Consider for atypical or young presentation
- Vasomotor (hot flash) symptoms predominate
- Vaginal pH
- pH > 4.5 indicates Menopause
- Women without Vaginitis and not receiving HRT
- pH <4.5
- Can be used to monitor for adequate HRT response
- References
- pH > 4.5 indicates Menopause
V. Diagnosis
- Serum FSH level are not necessary in age over 45 years
- Perimenopause: Hot Flashes and irregular Menses
- Menopause: Hot Flashes and no Menses for 6 months
VI. Management: General Approach
- See Health Concerns in the Elderly
- See symptom management below for Menopause and Perimenopause
- Osteoporosis Prevention
- See Osteoporosis and Osteoporosis Management
- See Fall Prevention in the Elderly
- Calcium Supplementation at 1200 mg per day
- Vitamin D Supplementation 800-1000 IU per day
- Cardiovascular Disease Prevention
- Postmenopausal women have a higher Incidence of Angina and worse CAD outcomes than men
- Postmenopausal women have a higher Incidence of Heart Failure with Preserved Ejection Fraction (HFpEF)
- Reduce CVA, HFpEF, CAD Risk by controlling Hypertension, Atrial Fibrillation, Diabetes Mellitus, Tobacco abuse, Obesity
- See Cardiac Risk Management
- See Exercise in the Elderly
- Tobacco Cessation
- Cerebrovascular Disease Prevention
- Manage Hypertension
- Manage Atrial Fibrillation
- Cancer Prevention
- Immunizations
- Influenza Vaccine annually
- Herpes Zoster Vaccine for 1 dose routinely at age 60 years
- Pneumococcal Vaccine routinely at age 65 years (Prevnar 13 and after 1 year, Pneumovax 23)
- Tetanus Vaccine (Tdap for at least 1 dose after age 19, then Td every 10 years)
- Sexual health
- Women are sexually active at least once weekly in >65% of cases
- Sexually Transmitted Infection occurs in at least 1% of women over age 65 years
- Psychosocial Concerns
VII. Management: Menopausal Symptom Management (and Osteoporosis Prevention)
- See Vasomotor Symptoms of Menopause
- See Atrophic Vaginitis
- Estrogen Replacement Therapy
- Weigh risks (CAD, DVT, CVA, Breast Cancer) versus benefits (Osteoporosis, Hot Flashes)
- Consider for women under age 60 years old or within 10 years of Last Menstrual Period
- After this, with advancing age, risks of CVA, MI, Dementia outweigh benefits
- See Cardiac Risk Management
- See Estrogen Replacement for a general overview of risks, benefits and protocols
- Estrogen Replacement is recommended only for symptom control (e.g. Hot Flushes)
- ACOG and AAFP do not recommend Hormone Replacement for chronic disease prevention
- (2013) Obstet Gynecol 121(6): 1407-10 [PubMed]
- Manson (2013) 310(13): 1353-68 +PMID:24084921 [PubMed]
- See Specific Estrogen Replacement Options
- Weigh risks (CAD, DVT, CVA, Breast Cancer) versus benefits (Osteoporosis, Hot Flashes)
VIII. Management: Perimenopausal Symptom management
- See Vasomotor Symptoms of Menopause
- Agents
- Provera 5-10 mg for 12 days per month
- Prevents Endometrial Hyperplasia
- Oral Contraceptives (OCP)
- Choose continuous low Estrogen option (e.g. Lo Loestrin Fe)
- Levonorgestrel IUD (Mirena)
- Stops Menstrual Bleeding but risk of atrophy
- Sequential Hormone Replacement
- Risk of pregnancy (HRT doses are much lower than OCP doses and inadequate for Contraception)
- Provera 5-10 mg for 12 days per month
- Evaluating end of Perimenopause for women on OCPs
- Identify when to switch to post-Menopause management
- Precaution
- Estrogen Replacement dosages are much lower than OCP doses and do NOT prevent pregnancy
- For women using OCPs for Contraception, transition to Estrogen Replacement should be carefully planned
- Protocol 1: Obtain Serum FSH on 6th day of OCPs Placebo pills
- Menopause suggested by FSH > 30 IU/L
- Protocol 2: Obtain Serum FSH and Estradiol level 2 weeks after stopping Oral Contraceptives
- Menopause suggested by a rise in FSH and no increase in Estradiol
- Castracane (1995) Contraception 52(6): 371-6 [PubMed]
- Protocol 3: Age based
- Likely safe to transition from OCP to Estrogen Replacement in mid-50s
- Allen (2013) CMAJ 185(7): 565-73 [PubMed]
IX. Management: Adjunctive Therapy
- Precaution
- This is controversial and not generally recommended due to potential for adverse effects
- Consider Androgen Replacement in Women
- Testosterone Replacement in Women
- DHEA Replacement in Women
- Combination Preparations
- E2P4T (Estrogen, Progesterone, Testosterone)
- Available from compounding pharmacies
- DHEA-S (see DHEA-S Replacement in Women)
- Used with the E2P4T
- E2P4T (Estrogen, Progesterone, Testosterone)
X. Management: Other agents
- See Vasomotor Symptoms of Menopause
- New agents
My Notes:
The Stages of Reproductive Aging Workshop STRAW+10 defines:
- Early menopausal transition (stage –2): persistent difference of 7 days or more in the length of > = 10 consecutive cycles
- Late menopausal transition (stage –1): amenorrhea for 60 days or longer
- Early postmenopause (stages +1a, +1b, +1c):
- Stage +1a lasts for 1 year after FMP and marks the end of perimenopause
- During stages +1a and +1b, lasting approximately 2 years after the FMP, vasomotor symptoms are most likely to occur.
- Late postmenopause (stage +2): Hormonal levels stabilize during this stage. Urogenital and vaginal symptoms typically become more prominent.
- Induced menopause: surgical bilateral oophorectomy, radiation/chemotherapy ablation
- Premature menopause: age of 40
- Early menopause: menopause before age 51
- Premature ovarian failure (POF): age 40
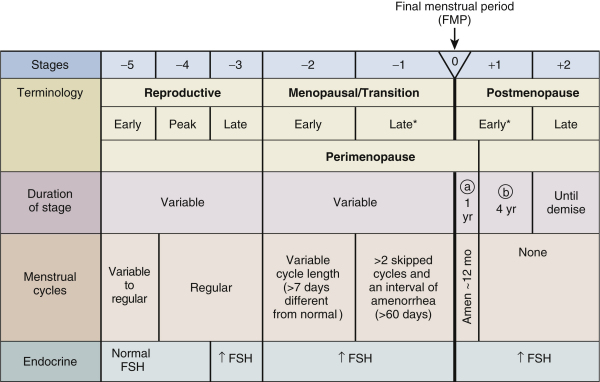
, the stages of the menopausal transition range from
[–2 or early menopausal transition to –1 or late menopausal
transition. The term perimenopause is similar and
often used interchangeably with menopause transition.
However, perimenopause generally encompasses at least
1 year postmenopause as well as the time leading to the FMP (Final Menstrual Period)
XI. References
- Shuer (2001) CMEA Medicine Lecture, San Diego
- Baill (2017) Am Fam Physician 95(9): 561-70 [PubMed]
- Greenblatt (1972) J Am Geriatr Soc 20:49 [PubMed]
- Hill (2016) Am Fam Physician 94(11): 884-9 [PubMed]
- Orentreich (1984) J Clin Endocrinol Metab 59:551 [PubMed]
- Seeman (1997) Am J Psychiatry 154:1641-7 [PubMed]
- Shifren (2000) N Engl J Med 343:682-8 [PubMed]
